Home »

CrescentCare featured in HRSA’s 2023 Ryan White HIV/AIDS Program Biennial Report
The following is excerpted from the full 2023 Ryan White HIV/AIDS Program Biennial Report, which can be downloaded here.
A Comprehensive Approach to HIV Care in New Orleans: CrescentCare

Originally founded in 1983 as the NO/AIDS Task Force to respond to the devastating effects of the AIDS epidemic in the New Orleans area, CrescentCare is a Federally Qualified Health Center (FQHC) and RWHAP Part D recipient and is also funded by Parts A, C, and F.
CrescentCare offers a range of services to the community, including people with HIV, in two locations in New Orleans and one in nearby Houma, Louisiana. Each year, CrescentCare serves more than 13,500 clients of all ages. Approximately 3,000 CrescentCare clients are people with HIV, of whom more than 2,800 are also RWHAP clients. Most of CrescentCare’s RWHAP clients are Black/African American (63 percent), and approximately 10 percent are Hispanic/Latino. Additionally, 6 percent of CrescentCare’s clients are people who are transgender, nonbinary, or genderqueer. CrescentCare’s Part D program serves 847 clients with HIV, most of whom are Black/African American.
CrescentCare offers primary and specialty medical care, behavioral health services, and medical case management to women, infants, and children living with HIV through
its Part D funding. The organization also offers housing assistance, syringe services, legal services, a food pantry, and other assistance to support clients with HIV, funded through other Parts of the RWHAP. Alice Riener, Chief Executive Officer, emphasized the importance of the comprehensive services provided by CrescentCare: “Since the organization’s founding, our approach has always been very broad and included an understanding that it requires more than just a doctor for people to be healthy.”
Reducing Health Disparities and Health Inequities
As part of its values and mission to provide comprehensive and inclusive health care, CrescentCare addresses health disparities and barriers to care, such as systemic racism, lack of housing, stigma, and other SDOH. These factors can interact with and exacerbate each other; affect a client’s ability to access HIV care and treatment; and influence HIV-related health outcomes, such as viral suppression.
To identify and address potential barriers to care, new CrescentCare clients are assigned a case manager who completes a comprehensive biopsychosocial assessment and works with them on goals for their care and health.
After the assessment, clients are referred to the appropriate CrescentCare programs or to programs run by community partners. For example, a client who is unstably housed is referred to housing services. For help with issues related to their HIV status-such as discrimination, securing public benefits, or creating a will-clients are referred to CrescentCare’s legal services. Peer support also is offered to people with HIV to connect with others who have HIV to share their experiences and offer emotional support.
 Newly diagnosed people with HIV are referred to the CrescentCare Start Initiative (CCSI), a rapid-start program to initiate antiretroviral therapy (ART) within 72 hours of diagnosis and provide ART for 30 days. Rapid ReSTART, a program for clients who have not received HIV care for nine months, is also available. Katherine Connor, Director of HIV Services, explained how CCSI has helped address systemic racism and other biases often embedded in HIV care: “The Rapid Start program really helps with bias and equity because it is the same protocol , and it is not dependent on somebody’s housing status or funding.” To ensure retention in care and care adherence, CrescentCare linkage coordinators track the patients’ follow-up visits, viral loads, and viral suppression status and engage or reengage with them as necessary.
Newly diagnosed people with HIV are referred to the CrescentCare Start Initiative (CCSI), a rapid-start program to initiate antiretroviral therapy (ART) within 72 hours of diagnosis and provide ART for 30 days. Rapid ReSTART, a program for clients who have not received HIV care for nine months, is also available. Katherine Connor, Director of HIV Services, explained how CCSI has helped address systemic racism and other biases often embedded in HIV care: “The Rapid Start program really helps with bias and equity because it is the same protocol , and it is not dependent on somebody’s housing status or funding.” To ensure retention in care and care adherence, CrescentCare linkage coordinators track the patients’ follow-up visits, viral loads, and viral suppression status and engage or reengage with them as necessary.
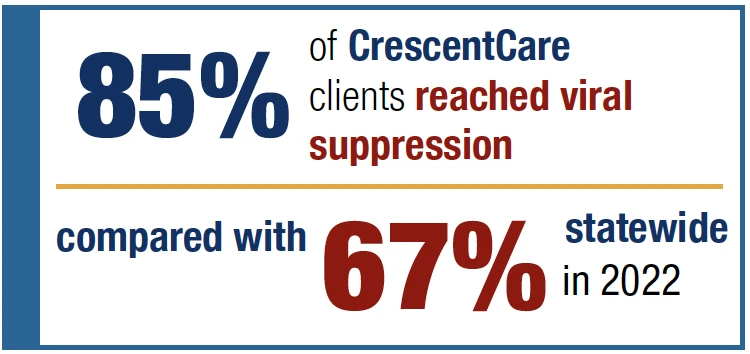
In 2022, CrescentCare patients with HIV had a viral suppression rate of 85 percent, compared with a statewide suppression rate of 67 percent. CrescentCare also addresses structural barriers to HIV care to ensure that it provides services that meet people where they are. Pamela Holm, Director of Primary Care, explained, “We do a lot of venue-based testing in the community at untraditional hours. We’re out at events. We have a mobile medical unit that goes out to reduce any sort of stigma from people coming in. We have bilingual staff to help with our Spanish-speaking population.”
Improving Health Outcomes With Access to Housing
In New Orleans, housing and homelessness are substantial challenges for many individuals, including people with HIV, and these problems are exacerbated by natural disasters like hurricanes and tornados. The housing crisis in New Orleans is also made worse by poor housing conditions-including mold, pests, and plumbing and electrical issues-that are present in almost 80 percent of New Orleans rental units.
Housing status is one of the strongest predictors of health outcomes for people with HIV. “The research certainly bears this out when you’re talking about social determinants of health and structural interventions that impact people’s health,” Riener explained. Individuals who are unstably housed are less likely to receive and adhere to ART; have lower CD4 counts and higher viral loads; and are more likely to have delayed entry into HIV care, be hospitalized, or require emergency care. “Here in New Orleans,” added Riener, “it’s very hard for our doctors or nurses to be working on people’s health when [patients] don’t have a stable place to live.”
 To help clients secure stable housing, CrescentCare offers Short-Term Rent, Mortgage, and Utility Assistance; Permanent Housing Placement; and Tenant-Based Rental
To help clients secure stable housing, CrescentCare offers Short-Term Rent, Mortgage, and Utility Assistance; Permanent Housing Placement; and Tenant-Based Rental
Assistance (a program similar to housing vouchers) through the U.S. Department of Housing and Urban Development’s Housing Opportunities for Persons With AIDS grants.
CrescentCare also supplies landlords with funds to help clients pay the first month’s rent, housing deposits, or outstanding utility bills. CrescentCare’s Director of Client Services, Tara Managan, pointed out that CrescentCare’s housing efforts are seamlessly tied to other RWHAP services: “Anybody who is eligible for Part C or Part D funding gets assessed and evaluated and referred to any of our housing opportunities.”
In 2022, CrescentCare housing programs helped 447 clients maintain stable housing through the end of the year. Managan also shared that in their experience, people can focus on many other aspects of their life once housing is lifted as a barrier.
Responding to the Mpox Outbreak
Because CrescentCare already had an infrastructure and processes in place to handle COVID-19 testing and distribution of vaccines, the organization was able to expand services to respond to the outbreak of mpox (formerly called monkeypox) in 2022 by requesting and distributing vaccines allocated by HRSA. Connor noted
the unique challenges associated with mpox. For example, mpox-which is spread by prolonged physical contact with someone who is infected or an exchange of bodily fluids-had predominantly been detected in gay men and communities of color. Recognizing the vulnerable populations, the subsequent stigma associated with mpox, and the limited availability of the mpox vaccine, CrescentCare worked diligently to identify high-risk patients and focus resources where they would make the biggest difference.
As more mpox vaccines became available, CrescentCare held regular vaccine events at each of its locations. Vaccine availability and events were promoted through CrescentCare’s website, social media, and word of mouth, as well as by directly reaching out to clients. “We did want to open it up to the community and not just our patients,” explained Connor. “Once we got more supply, we were able to do more walk-in events, which really helped to eliminate barriers.” Mpox vaccine clinics were held on weekends and early in the evening to ensure that services were accessible to the community. In total, CrescentCare vaccinated 2,426 clients.
In response to the stigmatizing and confusing information circulating about the virus, CrescentCare developed a comprehensive guide to mpox and its risk factors, which was distributed to the community on social media alongside information about the availability of the mpox vaccine.
In addition to holding its regular vaccine clinic events, CrescentCare prepared for Southern Decadence-an LGBTQ+ festival and parade that takes place annually in New Orleans over Labor Day weekend. The event is a celebration of diversity, inclusiveness, and LGBTQ+ culture that attracts thousands of people from around the world. CrescentCare, aware of the stigma surrounding mpox, held private vaccine clinics and reached out to patients via their primary care providers. As Connor noted, “For some people, getting it at their doctor’s visit was a more discreet way of doing it than some of the events at bars.” Following the Southern Decadence festival, CrescentCare also offered a vaccine clinic for people who were concerned about their potential exposure to mpox during the event. According to data from the Louisiana Department of
Health, no sustained increase in mpox cases was observed following the festival; Louisiana has averaged less than one mpox case per day since October 2022.
 Learning From the Past and Looking Toward the Future
Learning From the Past and Looking Toward the Future
CrescentCare is proud of the organization’s resiliency and accomplishments during the many challenges of the previous years, including COVID-19, Hurricane Ida, and mpox. Riener noted, “There are certainly several other organizations around the country that are HIV/AIDS service organizations that became Federally Qualified Health Centers. There are not very many of them operating in the Deep South in such resource-poor environments and in places that are being so directly negatively impacted by climate change.”
While the COVID-19 pandemic created obstacles to care, it also provided CrescentCare with opportunities to expand services. The medical and behavioral telehealth services that were quickly established at the beginning of the pandemic were so successful that they have continued even after in-person care was reinitiated. Telehealth services enable many clients to access care without having to miss much time from work or leave their homes. According to Managan, “Without telehealth services, patients had to choose: Do I go to work and make money to support myself and have food and housing and everything else, or miss work for an appointment?”
In summer 2020, CrescentCare’s leadership embarked on a series of conversations about how the organization could embed racial equity as a value into every aspect of the way it delivers services. With staff members serving as a steering committee, CrescentCare has been working with Beloved Community, a Black-led nonprofit, to develop a work plan to enhance racial equity within the organization. Feedback is being obtained from both staff and clients, and CrescentCare has been implementing components of the work plan, such as conducting trauma-informed training for supervisors.
Published: Oct 20, 2023



